VASCULAR CENTER
Vascular & Endovascular Surgery
Abdominal Aortic and Iliac Artery Occlusive Disease
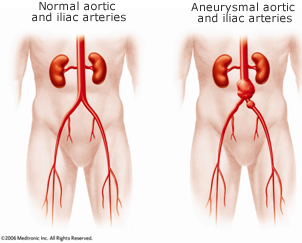 Abdominal aortic and iliac artery occlusive disease occurs when the arteries in your abdomen become narrowed with plaque and cannot bring enough blood to organs and muscles in your legs. There may be adequate blood flow through the artery to provide enough oxygen to the muscles when you are resting. But the muscles need more oxygen during activity, and if they can’t get enough blood, your legs may cramp or feel tired when you are walking or performing other tasks.
Abdominal aortic and iliac artery occlusive disease occurs when the arteries in your abdomen become narrowed with plaque and cannot bring enough blood to organs and muscles in your legs. There may be adequate blood flow through the artery to provide enough oxygen to the muscles when you are resting. But the muscles need more oxygen during activity, and if they can’t get enough blood, your legs may cramp or feel tired when you are walking or performing other tasks.
When plaque, which is made primarily of cholesterol and fatty acids with associated inflammation, builds up in your arteries, you have the condition known as atherosclerosis. As atherosclerosis progresses, the aortic artery can be completely blocked by plaque or by a blood clot lodged in a narrowed section. When this happens, the tissues below the blockage will not receive enough blood or oxygen, and will eventually die, causing a condition called gangrene. One symptom of this is cramping or pain in your leg when you are resting it.
If you have atherosclerosis, all your arteries, including those that carry blood to the heart muscle or brain, may also be affected. This puts you at risk of heart attack or stroke.
What Causes Aortic and Iliac Artery Occlusive Disease?
There are multiple factors that increase the risk of developing atherosclerosis that can cause aortic and iliac artery occlusive disease. The more risk factors, the greater the severity of the disease. The most common risk factors include:
- Cigarette smoking
- Diabetes
- High cholesterol or a high fat diet, or both
- Hypertension (high blood pressure)
- Age over 60
Family history
Symptoms of Aortic and Iliac Artery Occlusive Disease
- Cramping or aching in your hip, buttocks, thighs, or calves after a short walk. This pain is called claudication. The pain goes away when you stop the activity, but returns when you move again.
- Pain in your hip, buttocks, thighs, or calves that increases when you climb stairs or go uphill.
- Pain in a limb when you are resting. This is a symptom of severe arterial blockage.
Diagnosing Aortic and Iliac Artery Occlusive Disease
The three main components of diagnosing abdominal aortic occlusive disease are a history and physical exam by the doctor, a study of your blood flow in the vascular laboratory, and an imaging study called an arteriogram, which will pinpoint where the problems are.
History and Physical
The doctor will ask you numerous questions about your symptoms and determine any risk factors you may have for arterial disease. Try to be specific and mention all your concerns, even if you don’t think they are related: they could reveal an underlying symptom. List all your medications, including aspirin, blood thinners, and over-the-counter supplements.
Plaque can form in blood vessels throughout your body. For that reason, your doctor will feel for pulses and listen to the blood flow in your major arteries. Your abdomen, feet, and legs will be examined carefully for signs of arterial disease, which include changes in your nails, changes in skin color and temperature, and sores that will not heal.
Vascular Lab Tests
A vascular lab technician will check the blood flow in your abdomen, legs, and feet. The following are quick and painless tests that can confirm that there is inadequate blood flow to your legs, which is also called peripheral artery disease (PAD):
- An ankle-brachial index (ABI) is a series of blood pressure readings that compares the blood pressure in your ankle and foot with the blood pressure in your arm.
- Doppler ultrasound, which looks at the blood flowing through your arteries. It can show changes in blood flow due to narrowing or blockage of an artery.
Arteriography
If you are diagnosed with arterial disease, your doctor will send you for an arteriogram to show the amount of damage in an artery and its exact location. This test may only take a couple hours and is usually done on an outpatient basis, but with recovery time you should allow a full day.
Before the procedure, you’ll be given medication to make you comfortable. After the area is numbed, a long, thin tube called a catheter will be inserted into an artery, usually one of the femoral arteries, through a small puncture in one of your groins. The doctor will carefully thread the catheter through the affected artery, and once it is in place, will inject a contrast dye. The dye shows up clearly on the X-rays, to pinpoint where the artery is narrowed or blocked. After the procedure, you will be monitored while you keep your leg straight for several hours, but most patients resume their normal activities the following day.
Treatment of Aortic and Iliac Artery Occlusive Disease
There are some steps you can take to reduce the arterial damage caused by atherosclerosis. They include:
- Stop smoking right away.
- Use a thrombolytic or fibrinolytic drug as prescribed by your doctor to dissolve clots and relieve the pain of claudication.
If you have severe abdominal aortic occlusive disease, particularly if it does not improve with the measures described above, your doctor may recommend a minimally invasive endovascular treatment to improve the circulation in your legs. If your blockage is more extensive or cannot be treated with an endovascular procedure, bypass surgery may be required.
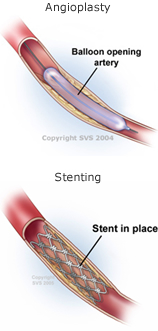 Angioplasty and stenting are endovascular procedures that may be used to repair a severely narrowed artery or a short blockage. Both can be done through a small puncture, usually at the groin. As a result, general anesthesia isn’t needed, so recovery can be much quicker and complications fewer than with open bypass surgery.
Angioplasty and stenting are endovascular procedures that may be used to repair a severely narrowed artery or a short blockage. Both can be done through a small puncture, usually at the groin. As a result, general anesthesia isn’t needed, so recovery can be much quicker and complications fewer than with open bypass surgery.
Angioplasty uses a tiny balloon to open blocked arteries. The balloon is inflated and deflated several times to press the plaque against the artery wall. Once the artery has been unblocked, the balloon is deflated and removed. Blood can flow freely through the widened artery.
Stenting is the insertion of a tiny wire mesh tube into an artery to hold it open. The collapsed stent is mounted onto a balloon catheter and guided across the blockage. The balloon is inflated to open the stent, which locks into place inside the artery. The balloon is deflated and removed, leaving the stent in place, holding the artery open.
