PATIENT INFORMATION
Abdominal Aortic Aneurysm Surgery
Procedure Instructions
Preparing for Surgery
- Stop smoking right away, it will help speed your recovery from surgery.
- You may want to donate your own blood ahead of time, for use during or after surgery, if needed.
- Tell your doctor about any medications you are taking, including over-the-counter supplements. Ask if you should stop taking them.
- Unless you are told otherwise, do not eat or drink anything after midnight on the day before surgery.
During surgery, the weakened aortic wall is replaced with a graft, which is a synthetic tube made of strong fabric. This may be done by either open surgery or an endovascular procedure. The method depends on the size and location of the aneurysm and ultimately is decided by you and your doctor.
Open Surgery for Aneurysm Repair
 A large incision is made along the abdomen. Once inside, your surgeon gently moves aside your organs to reach the damaged section of the aorta.
A large incision is made along the abdomen. Once inside, your surgeon gently moves aside your organs to reach the damaged section of the aorta.
- The aneurysm is then opened and cleaned to remove any clotted blood, if needed.
- The graft is sewn to the aorta at one end and to the iliac arteries at the other end.
- The wall of the aorta is wrapped around the graft to protect it. The wall is then sewn up.
- The incision site is closed with sutures and/or staples.
Endovascular Procedure/Endoluminal Graft Repair
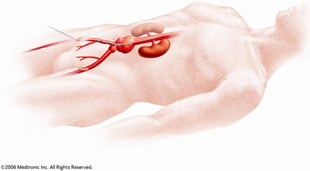 This is a new, minimally invasive approach to repairing an aneurysm. Rather than a large incision, you have several small incisions and your surgeon watches the procedure on a video monitor. This surgery provides a faster recovery with less pain.
This is a new, minimally invasive approach to repairing an aneurysm. Rather than a large incision, you have several small incisions and your surgeon watches the procedure on a video monitor. This surgery provides a faster recovery with less pain.
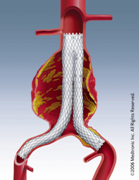
- One or two small incisions are made near your groin. Then a catheter (a thin, flexible tube) is threaded through an artery at each incision. A graft, or a section of a graft, is placed inside each catheter. The graft is guided toward the damaged part of the aorta.
- The catheter is used to place the graft in the correct position and the graft is expanded so blood can flow through.
- The graft is attached inside the artery above and below the aneurysm using metal springs called stents, and/or hooks.
- The catheter is removed and the incisions are sewn or stapled together.
After the Surgery or Procedure
After the operation, you will be taken to a recovery area where you will be watched closely. Once you are stable, you will be taken to the intensive care unit or to your room on the post-surgical floor.
Your nurse or a physical therapist will help you get up and walk soon after surgery. This will help your circulation and bowel function return to normal. It also helps to reduce swelling, promotes healing of your incision, and prevents lung problems, such as pneumonia. The sooner you are up and walking, the sooner you can go home.
You’ll be doing breathing exercises to make sure you are expanding your lungs completely. This may be uncomfortable at first but the exercises clear any fluid that may be in your lungs from surgery.
After Open Surgery
You can expect to be in the hospital for 5 to 10 days after an open AAA surgery. When you first wake up, you may feel groggy, thirsty, or cold. You will have a Foley catheter in your bladder, so you won’t need to use the restroom. For a few days, intravenous (IV) lines provide fluids and medications.
You may have a nasogastric (NG) tube from your nose to your stomach for a few days to keep your stomach empty until your colon starts to function again. Although an NG tube may be somewhat uncomfortable, it prevents nausea, vomiting, and other complications.
When you start to pass gas, it is a sign that your colon is working again and you’ll be started on a liquid diet. You will progress to a soft diet “as tolerated,” that means as long as you don’t experience nausea or vomiting. You will continue a soft diet for 2 to 8 weeks after surgery, depending on your healing, as ordered by your doctor.
After an Endovascular Procedure
You can expect to be in the hospital for 1 to 3 days after the endovascular procedure. When you first wake up, you may feel groggy, thirsty, or cold. You may have a Foley catheter in your bladder, and in that case won’t need to use the restroom. You may receive intravenous (IV) fluids and medications for a day or two. The doctor will instruct you about any dietary precautions.
Caring for Yourself after Surgery
When you and the doctor feel you are ready, you will be discharged from the hospital.
- Make sure you have a responsible adult to drive you home.
- Your doctor will instruct you on when to restart your medications. Take all medications as directed.
- When you return home, take it easy. Avoid strenuous activities. Don’t lift anything heavier than 5 to 10 pounds for at least 4 to 6 weeks after surgery. It is also common to have decreased energy for 2 to 3 months or longer, but try to keep as active as you can after that first 6 weeks, to re-build your strength.
- You can shower 24 to 48 hours after surgery unless your doctor specifies otherwise. It is O.K. to get the sterile tape on your incision wet, but do not soap it. Do not soak in a bath or hot tub until your incision is completely healed, which may be 6 to 8 weeks. If you have staples, you can shower without a bandage. Dry the area well afterwards.
Pain is common after surgery, especially around the incision site. The pain medication prescribed by your doctor will help with this pain, which should improve in the days following your surgery. Ask your doctor if you can take ibuprofen (Advil) between doses of your prescription pain medication, but do not take it if you are allergic to it, or if you have gastric ulcers or kidney problems.
Fever: A low-grade temperature is common after surgery. If your temperature exceeds 101.5 degrees or if it is accompanied by chills, vomiting, or flu-like symptoms, call the office.
Incision: When you leave the hospital, your incisions will be covered by a sterile bandage called a steri-strip. This will fall off or be removed when you have your post-op check. There may be some drainage from the incisions; this is normal. The drainage should be thin, watery, and slightly pink. It should not be bright red blood. Signs of an infection include thick green or yellow drainage, or skin around the incision that is red or warm to touch. Some swelling and bruising around the incisions is normal and should improve in the days following your surgery.
Diet: After open surgery your colon is adjusting due to a major operation. Constipation, diarrhea and poor appetite is to be expected for a few weeks. Try liquids and a soft diet for a few weeks. As you feel better, slowly move on to solid foods. Eat frequent, small meals to aid in digestion.
Nausea: Nausea is common after surgery. Be sure to take your pain medication on a full stomach. Stick to a soft bland diet for the first few weeks after surgery. If necessary, call your doctor and they can prescribe a medication to help with nausea.
Constipation: Constipation is very common following a surgery. The anesthetic used during the operation paralyzes the bowel, which can lead to constipation for up to a week. Pain medications such as Vicodin or Percocet also cause the bowel to move more slowly. You may try over-the-counter medications such as milk of magnesia, Colace, or Metamucil, as well as prune or apple juice to get your bowels moving.
When to Call the Doctor
- Fever over 101.5 degrees
- Increased redness or drainage from an incision
- Nausea or vomiting
- Persistent pain in the legs, abdomen, or back
- Difficulty breathing
When to Go to the Emergency Room
- Uncontrolled bleeding from the incisions
- Persistent vomiting
- Change in mental status
- Inability to breathe
You are always welcome to call the office with your questions or concerns. After hours, an answering service will direct your questions to the on-call providers. However, these individuals are unable to call in prescriptions for pain medication after 5 p.m.
